
The only pretreatment study was ATLANTIC 22 which showed no benefit in the composite primary end-points of infarct artery TIMI 3 flow and 70% ST segment resolution. ST elevation myocardial infarction (STEMI) Where fondaparinux is not available, then enoxaparin (1 mg/kg two times a day, subcutaneously) is preferred (class IB). 21 As a result, fondaparinux carries a class IA recommendation for pretreatment of NSTE-ACS but patients should receive UFH during PCI.
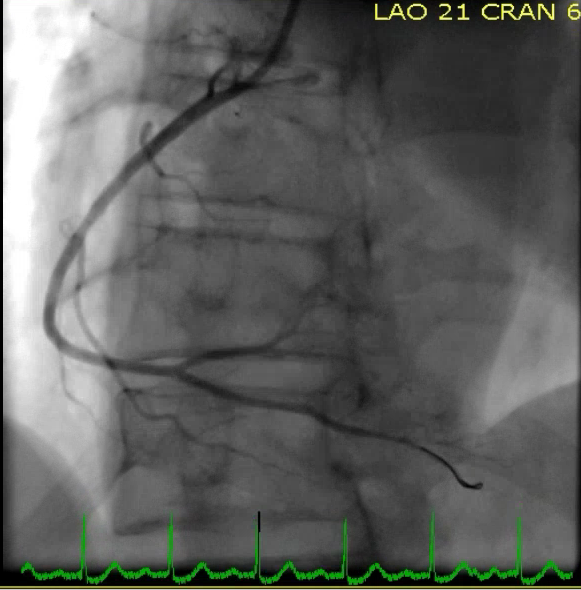
#Timi 3 flow. trial#
With respect to anticoagulants, the OASIS-5 trial showed equivalence of fondaparinux (2.5 mg od subcutaneously) to heparin in reducing composite events but with a reduced risk of bleeding. A non-randomised study of clopidogrel pretreatment (300 mg loading ≥12 hours or a 600 mg loading ≥2 hours before angiography) was associated with similar adjusted short-term ischaemic and bleeding outcomes compared with in-laboratory 600 mg clopidogrel loading (24 hours), antiplatelet pretreatment should be considered. Subsequent studies in NSTE-ACS were equivocal 4 10–12 showing no benefit of clopidogrel pretreatment. Non ST elevation acute coronary syndrome (NSTE-ACS)ĭata from PCI-CURE showed benefit of pretreatment with clopidogrel and aspirin in NSTE-ACS 9 both before and after PCI, even though the median time from randomisation to PCI was 10 days-in contrast to contemporary recommendation for early referral and invasive management (within 48 hours). There is no role for preprocedural anticoagulants. If coronary anatomy is known (or high probability of PCI) then pretreatment with clopidogrel (600 mg) at least 2 hours before procedure is recommended. In summary, for stable angina when coronary anatomy is not known, the evidence does not support pretreatment over in-laboratory loading with clopidogrel. Its use should be limited to high-risk patients unable to take oral medication. The CHAMPION-PHOENIX trial (included stable and unstable patients) found cangrelor to significantly decrease the combined primary efficacy endpoint and stent thrombosis within 48 hours compared with clopidogrel in P2Y12 inhibitor naïve patients undergoing PCI 7 without increase in severe bleeding. Cangrelor is approved but has not been tested in the pretreatment setting against in-laboratory clopidogrel. There is no evidence of patient benefit for glycoprotein inhibitors (GPI) in pretreatment. 6 Neither prasugrel nor ticagrelor have been tested in patients with stable angina. The absence of benefit from pretreatment loading is reflected in guidelines: The European Society of Cardiology (ESC) giving a IIb C recommendation for pretreatment loading only ‘if high chance of PCI’ 5 and the American Heart Association/American College of Cardiology (AHA/ACC) questioning its benefit without giving a recommendation. 3 The study finding was consolidated by a meta-analysis showing no mortality benefit from pretreatment. The only trial designed to test pretreatment was PRAGUE-8 which failed to show ischaemic benefit between prehospital 600 mg clopidogrel compared with in-laboratory treatment but with a higher risk of minor bleeding.
However, closer analysis of patient inclusion revealed that most were selected after coronary angiography. The evidence for pretreatment arose from the CREDO trial 2 which demonstrated benefit if patients received clopidogrel 300 mg loading at least 6 hours before PCI. Primary endpoint: all-cause mortality, MI, stroke or ischaemia-driven target lesion revascularisationħ119 patients at HBR or high ischaemic riskĭeath from any cause, non-fatal MI, or non-fatal stroke Rivoraxaban 2.5 mg two times a day+Aspirinġ month of DAPT followed by aspirin alone Net clinical benefit: 15% reduction in Ticagrelor arm Subgroup of THEMIS patients who underwent PCI Stable CAD and type 2 diabetes, no history of previous MI/Stroke ACS in previous 1–3 years with high ischaemia riskĪspirin+Ticagrelor 60mg two times a day vs


 0 kommentar(er)
0 kommentar(er)
